Enhancing the provider experience can improve access to care and encourage more providers to participate in Medicaid. A key facilitator of this is the transition to a modular Medicaid ecosystem that enables State Medicaid Agencies (SMAs) to effect change in policy, process, and technology to address provider experience challenges. The shift to modularity allows SMAs to avoid simply replacing their Medicaid Management Information System (MMIS) provider functions with a provider module that repackages the same flawed processes. Rather, agencies have an opportunity to evaluate and streamline the end-to-end provider experience. This approach seeks to reduces the administrative burden on providers by employing a provider-centric approach to process improvement and customer experience, ultimately freeing providers to focus on delivering quality care to their patients.
Unfortunately, Medicaid providers are unable to singularly focus on care or even remain in business due to time-consuming administrative burdens. While SMAs have their own set of challenges related to provider management, Medicaid providers experience pain points with enrollment, prior authorization (PA), and lack of clarity in how to resolve payment issues. Addressing provider experience pain points can benefit SMA staff as well the provider community.
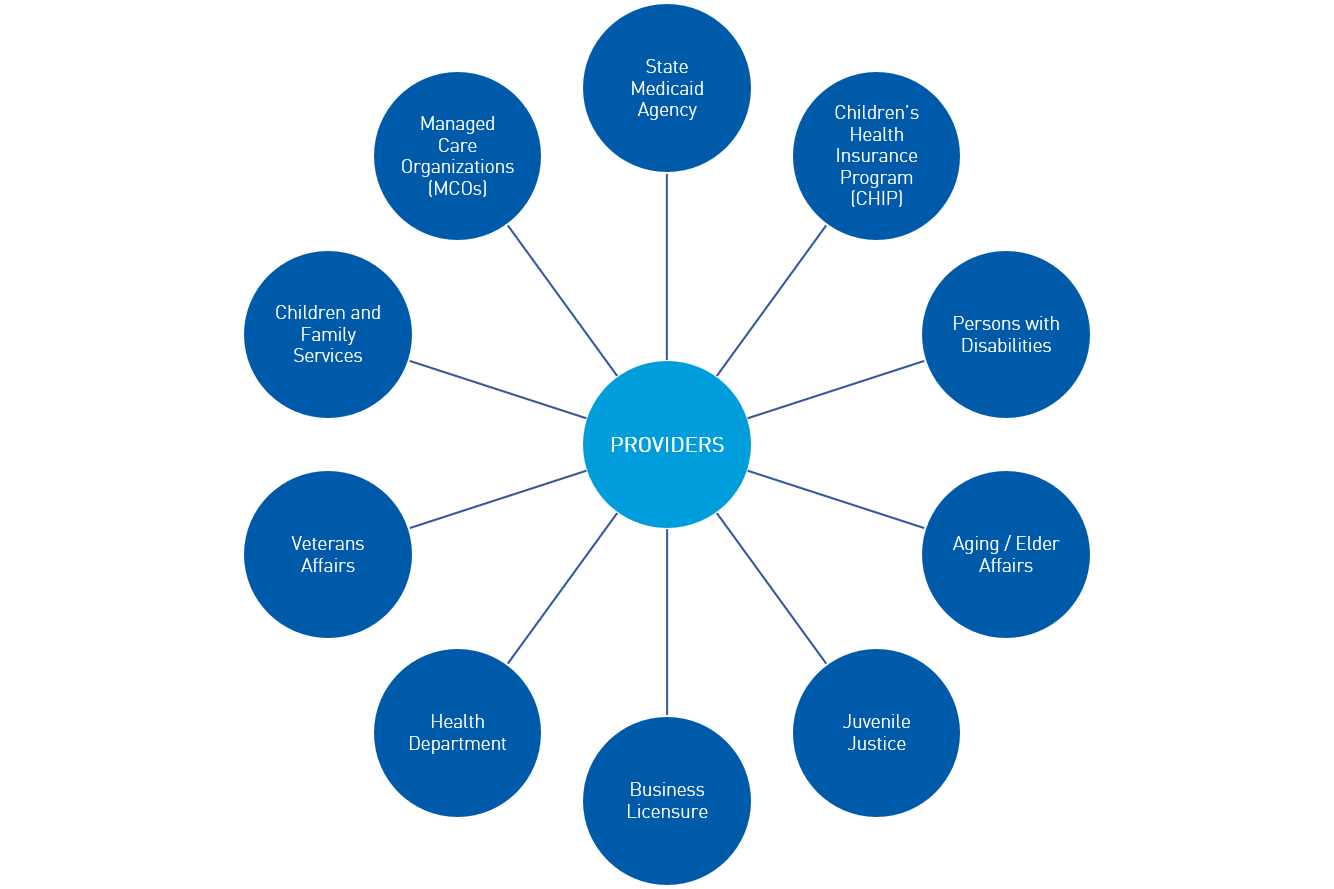
Before they're eligible to participate in Medicaid, providers today experience a cumbersome process. They’re required to navigate through multiple portals to enroll in Medicaid and separately credential with managed care organizations (MCOs). Even within an SMA, there could be multiple applications to complete. For example, facility regulation and licensure are often separate applications from Medicaid enrollment. If practicing in multiple locations, a provider must also manage separate Medicaid IDs, which can create its own challenges with enrollment and payments. Furthermore, providers also report supplying the same set of information to other state agencies within the Medicaid Enterprise.
A lack of consistency and transparency in PA rules across MCOs and Medicaid is another area of concern for providers. As a result, providers lack reliable means to understand which medications require prior authorization. Without a streamlined process to improve turnaround times for PAs and a clear path to escalate or appeal PA decisions, Medicaid providers will continue to face barriers to providing needed care, including avoidable payment denials.
Aside from the payment issues related to PA and provider identity reconciliation, Medicaid providers face a broader challenge of limited visibility into, and communications surrounding, payment denials. For example, even though fee-for-service (FFS) may only comprise a small percentage of the Medicaid population, FFS claims can account for a disproportionately large share of claims being processed due to repeat submittals of rejected or denied claims. Providers report having to submit the same claim numerous times because errors are identified and resolved one-by-one. Adding further confusion and frustration, providers also contend with long wait times for call centers and inconsistent responses from call center staff.
In order to address the full spectrum of challenges faced by providers, including enrollment, PAs, and payments, it is essential that SMA leaders take a people-centric approach. At North Highland, we apply design thinking techniques to guide our clients through visualizing and mobilizing new ways of thinking and doing, putting people at the center. To do this, we take a five-step approach that enables SMAs to transform the provider experience:
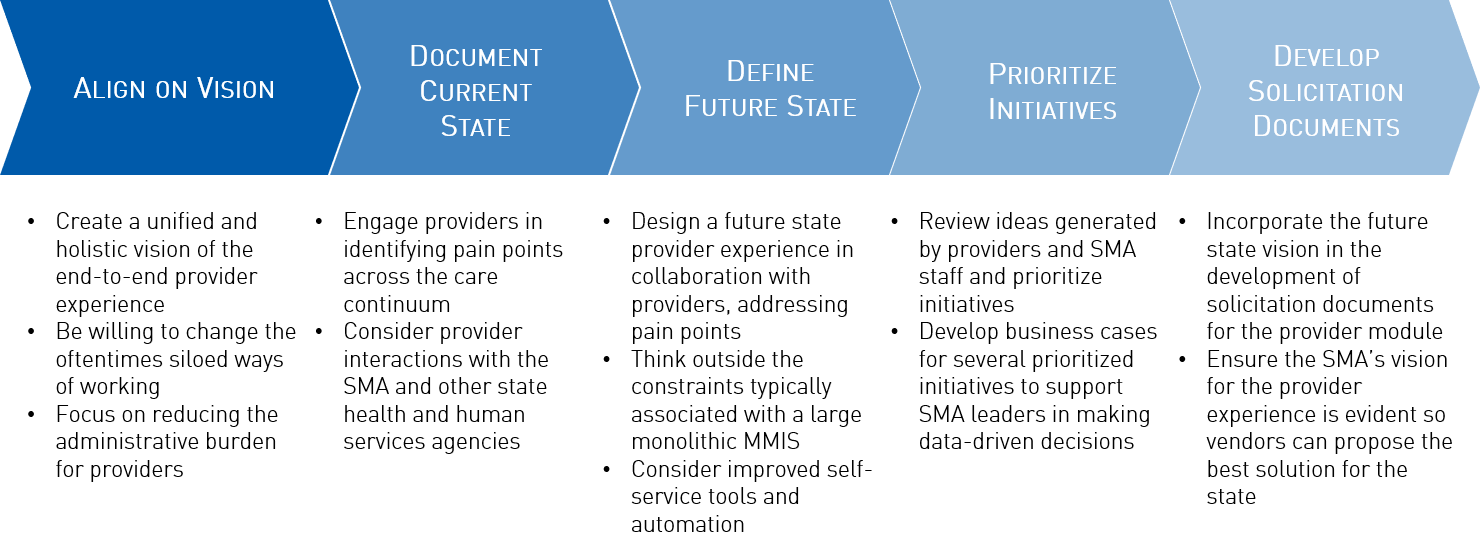
SMA’s efforts to improve the provider experience must be done in collaboration with providers, obtaining their feedback every step of the way. Engaging this key group of stakeholders in designing an improved provider experience will result in improved usage and adoption with the deployment of the provider module, as well as increased satisfaction among providers and SMA staff. Additionally, SMAs must consider lessons learned from commercial payors and Medicare in improving their provider experiences specifically related to provider enrollment and visibility into claim denials and prior authorizations. As with any improvement effort, it is important to assess both the tangible and intangible benefits against the costs of implementing these changes. SMAs on the path to modularity must be clear on their vision to ensure the functionality of their provider modules meet the needs of their providers for years to come.
